On October 13, 2023, the Centers for Medicare & Medicaid Services (CMS) released the 2024 Medicare Advantage Star Ratings. Here’s an in-depth look at 2024 Medicare Advantage Star Ratings, what changed, and how health insurers can improve their Medicare Advantage Star Ratings:
What Are Medicare Advantage Star Ratings
CMS developed Medicare Advantage Star Ratings to evaluate and compare Medicare Advantage (MA) plan performance. These ratings help beneficiaries make informed decisions when selecting a Medicare Advantage plan. But they also play a significant role in determining bonuses and quality-related incentives for MA plans.
The ratings range from 1 star (poor) to 5 stars (excellent), with half-star increments. CMS evaluates plans on several measures, and their overall rating is a weighted average of their performance across these measures.
What measures comprise the Star Ratings?
CMS rates Medicare Advantage with prescription drug (Part D) coverage (MA-PD) contracts on up to 40 unique quality and performance measures. For MA-only contracts (without Part D coverage), CMS reviews up to 30 measures. CMS evaluates Medicare Advantage prescription drug-only (PDP) contracts on up to 12 measures.
Star Ratings assess plans in several key performance categories, including:
-
- Staying Healthy: Measures related to preventive services, screenings, and immunizations.
- Managing Chronic (Long-term) Conditions: How well the plan helps members manage chronic health conditions.
- Member Experience: Beneficiary ratings of their experiences with the plan.
- Complaints and Changes in Plans: Includes how many complaints the plan receives and how often members switch plans.
- Customer Service: Evaluates how well the plan handles questions, solves problems, and provides information.
- Pharmacy Services: How well the plan delivers prescription drug services.
- Plan Responsiveness and Care: Addresses how quickly a plan provides care and addresses health concerns.
- Improving or Maintaining Physical and Mental Health: Focused on the health outcomes of plan members.
- Drug Pricing and Patient Safety: Assesses the affordability and safety of prescription drugs offered by the plan.
Star Ratings have financial implications for MA plans. Plans with higher ratings receive bonuses while beneficiaries choose highly-rated plans more frequently. They can also attract more beneficiaries because beneficiaries perceive higher-rated plans as offering better quality care.
Were Any Methodological Changes Made for 2024?
There were a few methodological changes that impact the 2024 Medicare Advantage star ratings:
- CMS transitioned The All-Cause Readmissions as a new measure into the 2024 Star Ratings with a weight of 1.
- CMS retired the Diabetes Care – Kidney Disease Monitoring measure.
- CMS added the Transitions of Care (Part C) and Follow-Up After Emergency Department Visit for People with Multiple High-Risk Chronic Conditions (Part C) measures, each weighing 1.
- The weight for the Part C Controlling Blood Pressure measure was increased from 1 to 3.
- CMS introduced the Tukey outlier deletion to the 2024 Star Ratings when calculating the cut points for all non-Consumer Assessment of Healthcare Providers and Systems (CAHPS) measures. Tukey outlier deletion removes outlier contract scores before applying mean resampling within the hierarchical clustering algorithm to determine measure-level cut points. We wrote more about this modification in an article titled The Future of Medicare Advantage Star Ratings.
What Happened to Ratings in 2024?
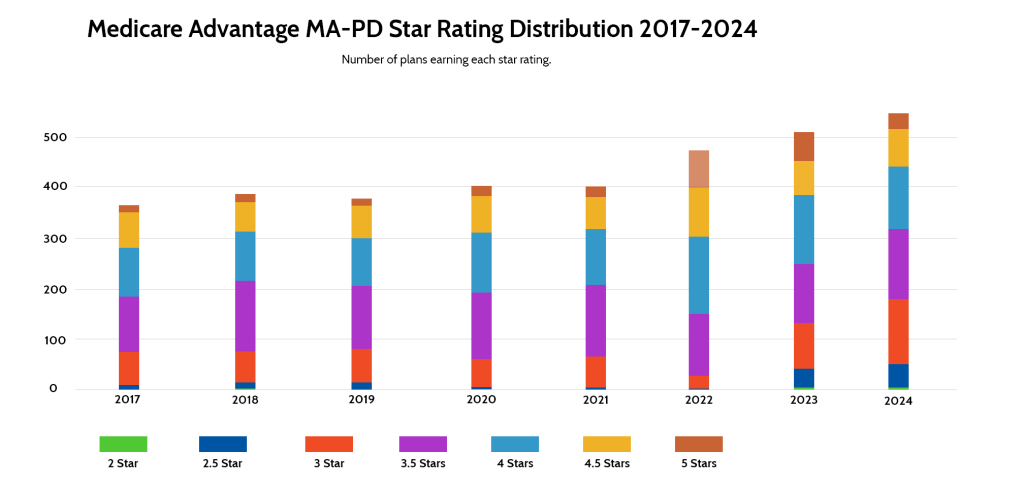
It’s becoming more difficult for Medicare Advantage plans to earn high Star Ratings. In 2022, nearly 16% of MA-PD plans earned five stars. That number dropped to just over 11% in 2023. In 2024, just 5.69% of MA-PD plans earned a five-star rating. In 2022, the average MA-PD plan earned a 4.37-star rating. That declined to 4.14 in 2023 and dropped further to 4.04 in 2024.
The percentage of plans earning four stars or higher also decreased. In 2022, nearly 70% of plans were rated four stars or higher. That dropped to 51% in 2023 and even further, to 42% in 2024.
Though the three-year trend is down, 2024 is similar to 2021, in which the average star rating was 4.06, and 5.25% of plans earned a 5-star rating. In 2021, 48% of plans were rated four stars or higher.
Do Non-Profit plans outperform for-profit plans?
Generally speaking, yes. 56% of non-profit MA-PD contracts received four or more stars, compared to 36% of for-profit contracts. That said, a greater percentage of for-profit plans earned the highest ranking of 5 stars – over 6%, compared to just under 4% for non-profit plans.
Do more experienced plans earn better Star Ratings?
Yes, more experienced plans outperform less experienced plans, on average. MA-PD plans with ten or more years of experience had a higher percentage of plans with four or more stars than contracts with less than five years of experience. Eight percent of those with more than ten years of experience attained five stars, compared to just under 3% for those with 5 to 10 years of experience and just over 3.5% for those with less than five years of experience.
What Individual Star Ratings Saw the Biggest Changes?
The Care for Older Adults – Medication Review and Renewing Appeals Decisions saw the largest decline among Medicare Part C Star Rating measures; both dropped from 4.4 to 3.8. Health Plan Quality Improvement experienced the biggest increase, improving from 2.6 to 3.0.
Among Part D measures for MA-PD plans, Call Center – Foreign Language Interpreter and TTY Availability experienced the most significant decrease, falling from a 4.4 average to a 3.7 average. Drug Plan Quality Improvement saw the greatest increase, from 2.7 on average to 3.4.
How can Health Plans Improve Star Ratings?
In the past, we wrote a Guide to Medicare Advantage Star Ratings that includes information about how to improve Medicare Advantage Star Ratings.
Certifi’s health insurance premium billing and payment solutions help Medicare Advantage payers improve member satisfaction while reducing administrative costs.