Last week, we answered the question “What are essential community providers?” This week, we’ll dig into another topic discussed in the Notice of Benefit Payment Parameters for 2023, network adequacy standards for qualified health plans (QHPs).
Here’s an overview of the history of network adequacy in healthcare and the potential impact of the 2023 Notice of Benefit Payment Parameters on health insurers who offer plans in the federal health insurance marketplace.
What are network adequacy standards?
Network adequacy generally refers to a health plan’s ability to provide reasonable access to in-network healthcare to a plan’s members. Generally, health insurers have narrowed their networks in an attempt to conserve costs, coordinate care or even exclude underperforming providers. That narrowing of networks may negatively impact a member’s ability to receive care.
As a result, states began to create laws designed to ensure that a health plan’s network is “adequate.” As early as 1997 states began to enact legislation that defined network adequacy requirements for health plans. For example, Montana enacted network adequacy standards in 1997 that set standards around ratios of providers to covered persons, geographic accessibility, waiting times, hours of operation, and more.
What impact did the Affordable Care Act (ACA) have on network adequacy?
The ACA created marketplaces individuals could visit to shop for insurance. That included a federal marketplace that many states used instead of a state exchange. For insurers to sell plans in these marketplaces, they need to meet several standards, including network adequacy. The ACA initially aimed:
- to ensure plans had a sufficient number of providers
- provide information to members and potential members about in-network and out-of-network providers
- include essential community providers within networks.
Final rules published in 2012 provided more color to these requirements. That included stating that the “network that is sufficient in number and types of providers, including providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”
Those standards were hard to quantify. As a result, the Obama administration in 2016 proposed enforcing quantitative standards for network adequacy. In a Letter to Issuers, the Centers for Medicare and Medicaid Services (CMS) created a table of maximum time and distance standards based on the area served. For example, in a large urban area, at least 90% of enrollees in a plan should be able to reach a hospital in 10 miles or 20 minutes. In a rural county, that was 60 miles or 75 minutes. However, the administration faced negative feedback during the comment period. That resulted in the administration backing off enforcement in the 2017 plan year. The Trump administration later released a Market Stabilization Final Rule in 2017. That rule shifted network adequacy oversight to states.
What changes did the 2023 notice of benefit and payment parameters have on network adequacy for qualified health plans?
Most significantly, the new proposed rule proposes that Health and Humans Services (HHS) will review the adequacy of Qualified Health Plan provider networks for plans in the federal health insurance exchange, except in states where the network adequacy rules are at least as stringent as the federal rules. Those reviews will be based on three types of network adequacy standards:
-
Time and Distance Standards
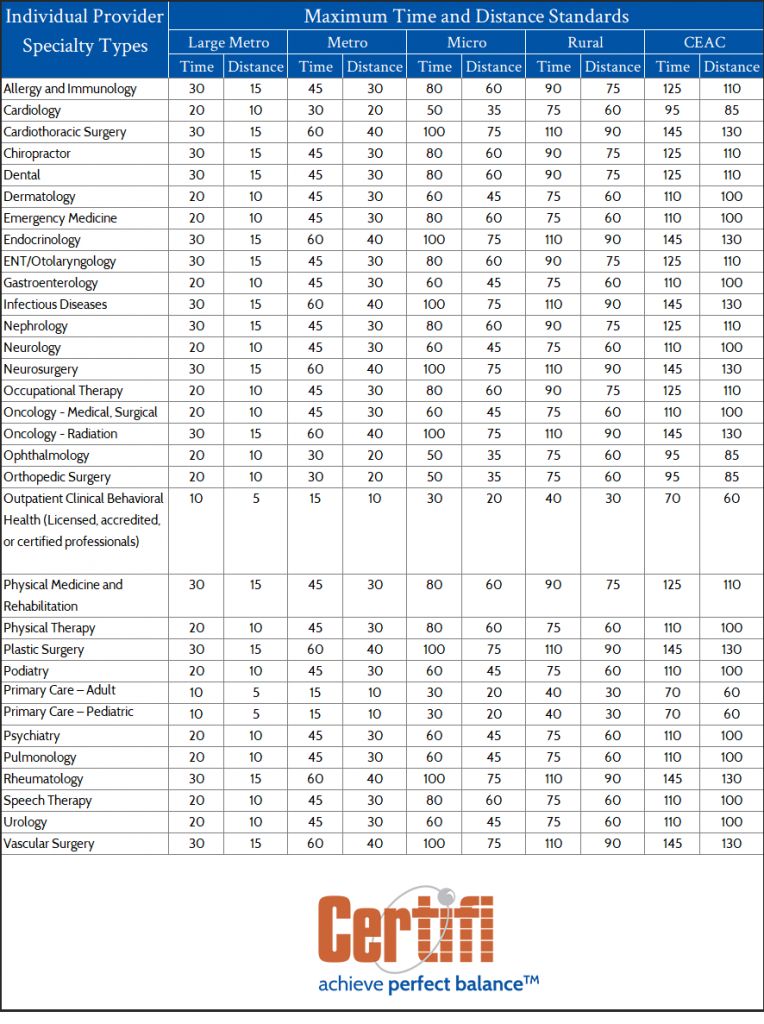
The goal of the time and distance standards is to make networks more robust, comprehensive, and responsive to enrollees’ needs. Though modeled after the Medicare Advantage network adequacy standards, the QHP standards include additional provider specialties. Overall, HHS proposes time and distance standards for 34 different individual provider specialties and 11 facility specialties. The department also proposes that the standards would be calculated at a county level and each county would be designated with a specific type based on its population and density. Those designations match Medicare Advantage designations — Large Metro, Metro, Micro, Rural, or Counties with Extreme Access Considerations (CEAC) and standards adjusted based on those designations. CMS released the actual time and distance parameters that QHPs need to meet in the 2023 Draft Letter to Issuers. We’ve provided the standards below.
Plans that fail to meet time and distance standards would be able to submit justification for any variances.
-
Appointment Wait Time Standards
Much like time and distance standards, the appointment wait time standards create categories under which appointment wait times would be measured. In this case, measurement occurs through three provider specialty categories: Behavioral Health Services, Primary Care (Routine), and Specialty Care (Non-Urgent). Like the time and distance standards, CMS released the specific appointment wait time standards in the 2023 Draft Letter to Issuers. We’ve provided the standards below. HHS proposes monitoring wait times through compliance reviews conducted after access to care complaints and through random sampling.
-
Tiered Network Standards
HHS also provided guidance for plans that have tiered networks. Those plans can satisfy the network adequacy requirements with providers contracted within the network that have the lowest cost-sharing costs. For example, some plans have preferred and participating providers, where the cost share is lower for preferred providers. Only preferred providers would count toward network adequacy standards.
Telehealth
Though no standards will be set, HHS would also like all certified QHPs to submit information about whether network providers offer telehealth services. Initially, the data will be used only for informational purposes but could be incorporated into standards in the future.
These proposed rules, which would first apply to plans in the 2023 plan year, are under comment until 5 p.m. on January 27, 2022. HHS considers those comments and then issues final rules codifying the proposed rules.
Certifi’s health insurance premium billing and payment solutions help healthcare payers improve member satisfaction while reducing administrative costs.