On February 29, 2024, the Centers for Medicare and Medicaid Services (CMS) released the Final Medicare Prescription Payment Plan (M3P) Part 1 Guidance. At the same time, it also released M3P model documents for six of the member forms and notifications related to the program. You can view those documents here: The Medicare Advantage and Prescription Drug Programs: Part C and Part D Medicare Prescription Payment Plan Model Documents.
Here’s a look at those Medicare Prescription Payment Plan model documents, including what they are and when plans should use them:
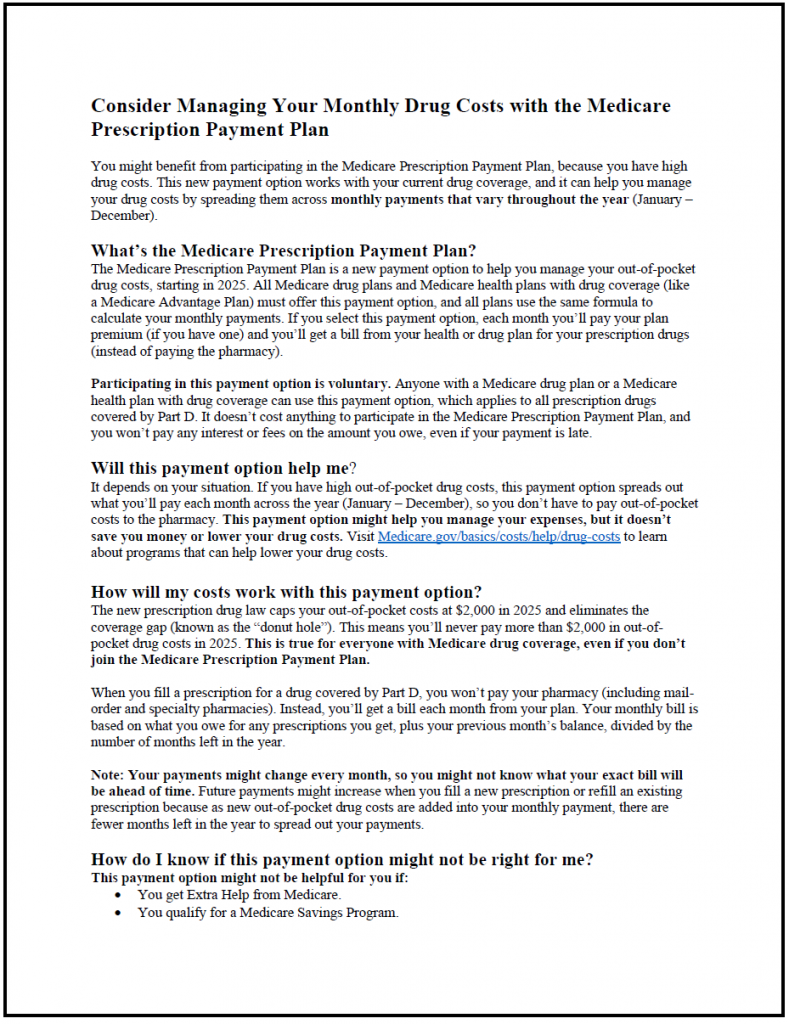
Likely to Benefit Notice
What It Is
Plan sponsors must identify members likely to benefit before and during the plan year. The Likely to Benefit Notice describes the M3P program, describes the monthly payment calculation, points to additional resources, and explains how to sign up for the program.
When It Is Used
Plans deliver the Likely to Benefit Notice to members identified as likely to benefit from the M3P program based on an analysis of prescriptions through September of the current year. The plan must send the Likely to Benefit Notice if the member incurred $2,000 in out-of-pocket costs through September. Plans must also send the communication if they become aware of any new high-cost prescriptions for an enrollee that would trigger a point-of-sale notification. The notification may be sent by mail or email, based on the member’s preference.
Plans must also supply the notice to pharmacies to distribute to those who meet the point-of-sale threshold, which CMS defined as a single $600 out-of-pocket prescription cost.
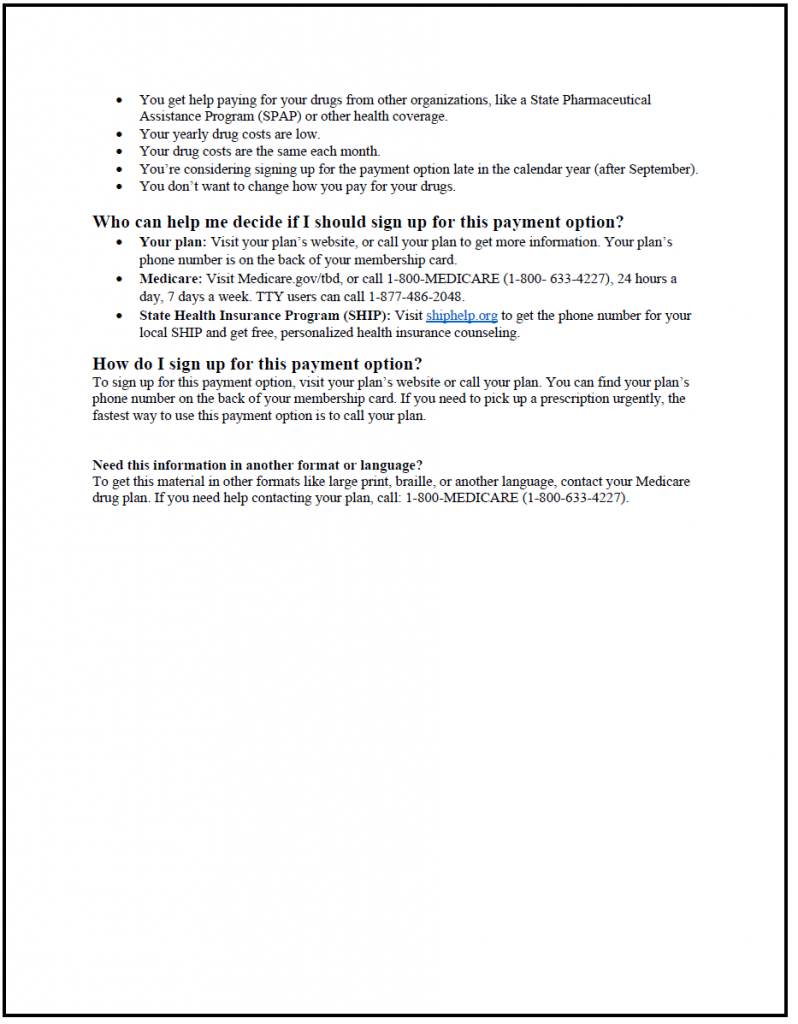
Participation Request Form
What It Is
A paper enrollment form Part D plans can use to enroll members.
When Is It Used
Plans can use the Participation Request Form at any time to enroll a member in the Medicare Prescription Payment Plan. Per the M3P guidance, all Part D enrollees must be able to enroll in the M3P program.
The form asks for basic information – like name, Medicare Number, phone, address, and whether a member gets help paying for prescription drug costs. The form also reserves space for plan-specific terms and conditions related to the Medicare Prescription Payment Plan.
Note that plan sponsors must have the following enrollment mechanisms available:
- Send a form as part of member card issuance
- Have available a paper form to mail to members
- Use a website application that captures member enrollment data as well as proof of enrollment
- A toll-free number that also captures enrollment information and proof of enrollment.
Election Approval Notice
What Is It?
The election approval notice is sent to members after they’ve enrolled. It confirms enrollment in the Medicare Prescription Payment Plan. It includes information about:
- M3P program’s next steps
- The monthly bill calculations
- What happens if the member fails to make a payment
- How to leave the M3P program
- Other programs that can reduce costs
When Is It Used?
If the M3P Election Approval Notice is received before the plan year, it must be sent electronically or by mail within 10 days of the election receipt or the number of calendar days before the plan enrollment starts, whichever is shorter. If the plan approves enrollment during a plan year, it must send the Approval Notice within 24 hours of the election request.
Failure to Pay Notice
What Is It
Plans use the Failure to Pay Notice to notify members that they didn’t pay their monthly Medicare Prescription Payment Plan payment by the due date. It informs a member that they must make a payment during the grace period and what happens if they fail to pay. It also includes information about how to pay, how to file a grievance, and programs members can use to lower prescription drug costs.
When Is It Used?
Plan sponsors must send the initial Failure to Pay notice within 15 days of the payment due date.
Termination Notice
What Is It?
The Termination Notice notifies members that the health plan has terminated their participation in the M3P program for failure to pay. It includes:
- That the plan terminated the member from the M3P plan (but not the Part D plan), and the termination date
- The member is still required to pay the amount owed
- The member must pay for prescriptions at the point of sale.
- How to pay the remaining balance
- How to file a grievance
- Once they pay their remaining balance, members may participate in the M3P program in the future
- Other programs to lower costs
When Is It Used?
Plans must send Termination Notices within 3 business days of the end of the grace period.
Voluntary Termination Notice
What Is It?
Plans send the Voluntary Termination Notice if a member chooses to opt out of the M3P program or if they change their plan. It includes information about:
- The effective date of the voluntary termination and that the member will now pay the pharmacy directly for out-of-pocket costs
- This termination only applies to the Medicare Prescription Payment Plan
- That the member may pay the balance all at once or monthly as billed, and how to make a payment
- What happens if a members does not make a payment
- How to enroll in M3P in the future
- Other programs that may reduce costs
When Is It Used?
Though the guidance doesn’t clearly state that plans must send Voluntary Termination Notices within a specified time period, we assume that like the Termination Notice, plans must send the notice within three days of the voluntary termination.
Certifi’s Medicare Prescription Payment Plan billing and payment solutions help Part D plan sponsors and PBMs save time and improve M3P billing accuracy.