Earlier this month, the Centers for Medicare & Medicaid Services (CMS) published their Medicare Advantage Star Ratings for 2023 plans. Here’s a breakdown of the Medicare Advantage Star Ratings for 2023:
What are Medicare Advantage Star Ratings?
CMS publishes Star Ratings for each health plan to help consumers compare Medicare Advantage quality among multiple plans. CMS uses a one to five-star scale to measure Medicare Advantage health plans. Three types of Medicare Advantage plans exist:
- Standalone Medicare Advantage – These plans don’t offer prescription drug coverage.
- Medicare Advantage with Prescription Drug Coverage – These plans offer Medicare Advantage coverage and prescription drug coverage.
- Standalone Prescription Drug Coverage – These plans only offer prescription drug coverage.
Did the Methodology for Medicare Advantage Star Ratings Change in 2023?
CMS evaluates each plan type by different measures that determine their overall star rating. In 2023, CMS used 38 quality and performance measures for Medicare Advantage with Prescription Drug Coverage plans, 28 measures for Standalone Medicare Advantage plans, and 12 for Standalone Prescription Drug Coverage plans.
CMS more heavily weighted patient experience/complaints and access measures for the 2023 Medicare Advantage Star Ratings. Additionally, CMS removed a provision related to the COVID pandemic that enabled health plans to use their best performance from current or previous years for most measures.
What happened to ratings in 2023?
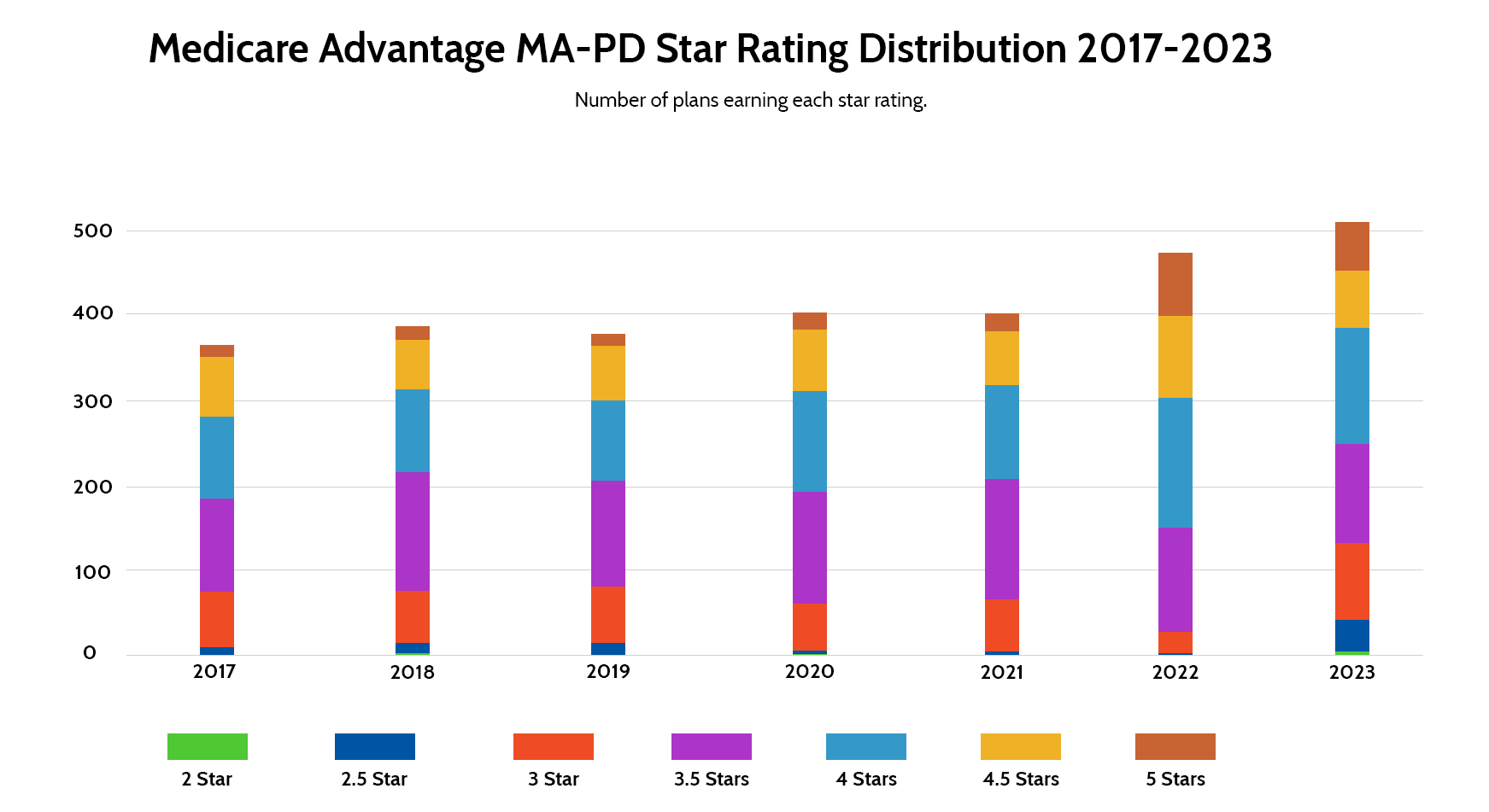
A significant decline in Medicare Advantage Star Ratings occurred in 2023. The average Medicare Advantage with Prescription Drug Coverage plan star rating dropped from 4.37 to 4.15. Nearly half of those plans achieved a star rating of 4 stars or greater, down from nearly 70% a year ago. From 2020 to 2022, just one health plan earned a 2-star rating, while four did in 2023 alone.
Standalone Prescription Drug Coverage plans saw similar declines. The average Prescription Drug Coverage plan earned a 3.25-star rating in 2023, down from 3.70 in 2023 and significantly lower than the three-year low of 3.5 in 2020.
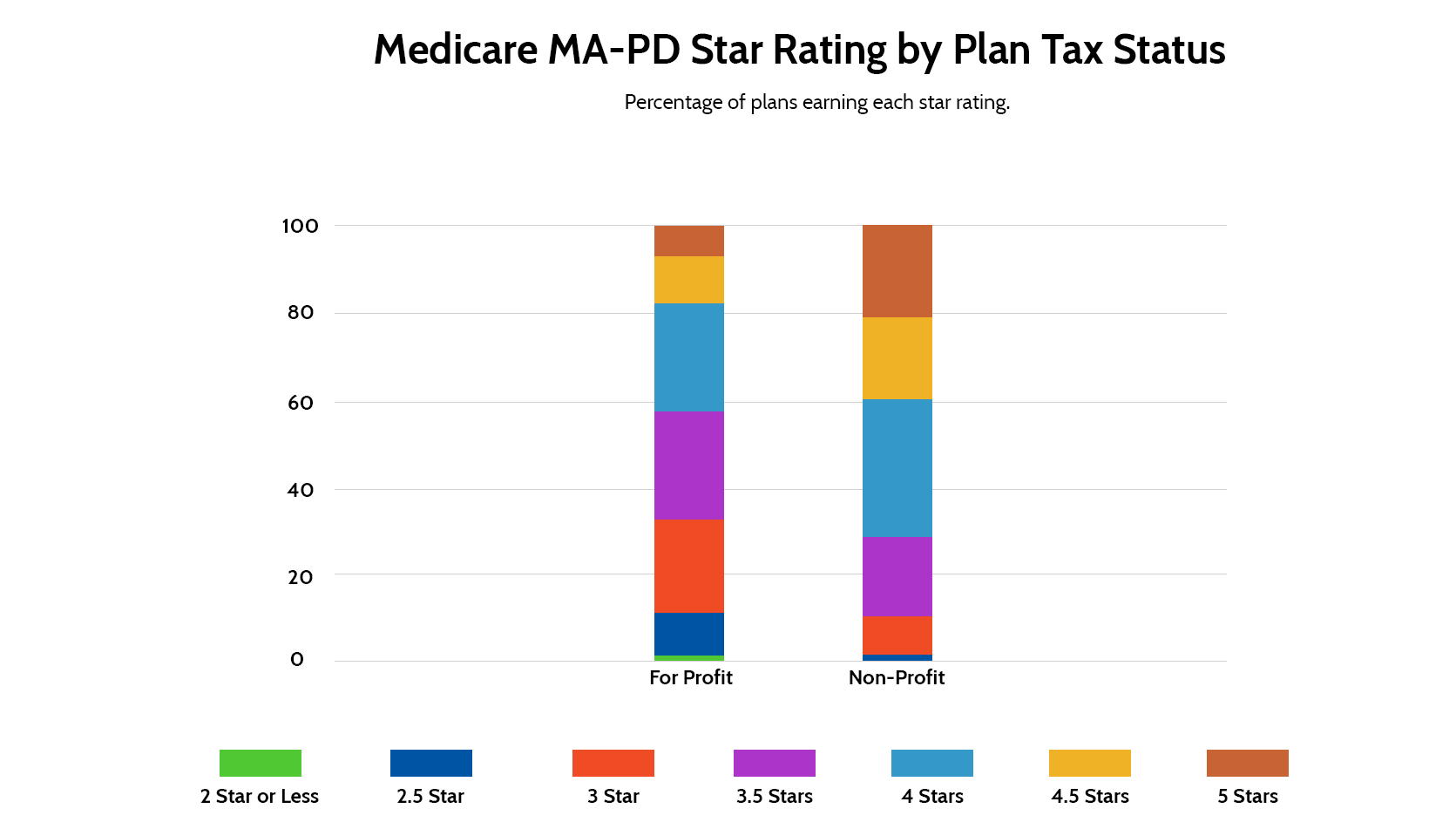
Non-profit plans performed better than their for-profit counterparts. Approximately 70% of non-profit Medicare Advantage with Prescription Drug Coverage health plans achieve a rating of 4 stars or better, compared to roughly 40% of their for-profit peers.
What individual Medicare Advantage Star Rating measures saw the most movement?
Individual measures that saw the largest increase and decrease from 2021 to 2023:
Improvements
- Osteoporosis management in women who had a fracture increased by 5.36 points.
- Diabetes care – blood sugar controlled increased by 2.57 points
- Statin use in persons with diabetes increased by 1.98
- Diabetes care – eye exam increased by 1.79 points
Deterioration
- Members choosing the leave the plan increased by 2.47 points for Medicare Advantage plans and 2.86 points for Prescription Drug Coverage plans, which is a negative outcome
- Call center – Foreign Language Interpreter and TTY Availability dropped by 2.22 points
- Reducing the risk of falling declined by 2.02 points
- Improving bladder control declined by 2.04 points
- Getting needed care dropped by 1.8 points
- Getting appointments and care quickly declined by 1.68 points
What is the Impact of Medicare Advantage Star Ratings on Health Plans?
Lower Medicare Advantage Star Ratings can impact health plan revenue. CMS uses star ratings to determine whether a health plan is eligible for quality bonus payments. Plans that achieve at least 4 out of 5 stars can have their benchmark increased. The benchmark is the amount that the federal government pays the health plan for each Medicare Advantage enrollee. Health plans typically see a 5% increase in that benchmark, though in some counties they may earn a 10% increase.
Additionally, CMS designed the Medicare Advantage Star Ratings to help consumers choose quality plans. As a result, consumers are more likely to select Medicare Advantage health plans with at least four stars. In 2022, for example, about 68% of health plans achieved a four-star or better rating, yet nearly 90% of enrollees enrolled in a four-star plan. Health plans earning four-star or better ratings receive revenue through an enrollment bonus and increased enrollment.
The decline in Medicare Advantage Star Ratings also impacted the health insurance markets in general. Both CVS Health and Centene stocks declined by nearly 10% when star ratings were released. Additionally, UnitedHealth Group, Cigna, Elevance Health, Alignment Healthcare, and Humana also saw their stock price decline on the day the Star Ratings were released, though only by 1% to 3%.
Certifi’s health insurance premium billing and payment solutions help healthcare payers improve member satisfaction while reducing administrative costs.